It’s been more than 20 years since Garry Kasparov lost his famous chess match against IBM’s Deep Blue, which heralded much anxious commentary about how humanity was soon to be subjugated by the superior processing power of supercomputers. Two decades later and our cultural understanding of AI can feel like it’s still stuck in the nineties.
Videos of increasingly agile robots from Boston Dynamics steal headlines about the AI-apocalypse, while AI’s application in other industries can be all but ignored by the mainstream.
However, amid all the worry about AI taking jobs, there’s little informed debate and nowhere is this more true than in healthcare. As far as the public perception of AI and health, we have struggled to move beyond the idea of robot doctors.
The reality of AI’s likely influence in health is more nuanced and, I’d argue, more exciting. The healthcare sector is already a key battleground in the coming AI revolution, with the AI health market expected to reach $6.6 billion by 2021. Jeff Bezos, Warren Buffett and Jamie Dimon have entered the market with much media attention, but can AI deliver the cost savings they seek while maintaining equal or better patient outcomes?
AI in healthcare: Strengths and limitations
It’s worth remembering that AI is a collection of different technologies, which together represent a real opportunity to improve efficiency in administrative and clinical healthcare practices. Take Moorfields Eye Hospital in London, the hospital has teamed up with Google DeepMind to greatly increase the detail at which they’re able to analyze retinal scans, opening up the potential for earlier diagnosis and cures of otherwise debilitating conditions. Meanwhile companies like BenevolentAI are using AI technology very differently, to rapidly accelerate the process of drug discovery.
At the other end of the scale, AI-driven chatbot technology is being used by Babylon Health to ease the burden on the UK’s National Health Service by offering basic diagnoses and appointment scheduling through smartphone apps.
But Babylon is a case in point of AI’s weaknesses as well as its strengths: the app got into trouble recently after finding that some users have been ‘overplaying’ their symptoms in order to get appointments faster. This cuts to a key weakness of AI in healthcare: while it’s great for analysis and research, healthcare still needs a human touch. How can we reconcile these two conflicting directions?
Lessons from chess
The key is in finding the right balance, and, as unlikely as it sounds, there are lessons from chess. After Garry Kasparov’s infamous defeat against IBM’s Deep Blue, he went on to consider the possibilities offered by playing chess in partnership with computers rather than against them.
Rather than admitting defeat, he invented a new form of the game, called Advanced Chess, where a human and AI work together. The brute force analysis of the computer system together with the more strategic thinking of the human player has taken the game to heights of skill never seen before, and it’s now an active sport around the world.
We need a similar approach in healthcare. It’s overly simplistic to see AI technologies and human medical professionals as opposed to each other in a battle over jobs. What matters most is patient outcomes, and a combination of strong AI-led analysis with a human context has the potential to deliver massive improvements.
While machine learning scanning technology is able to detect microscopic lesions or tumors on scans better than the human eye, this on its own is not enough. Healthcare is a multidisciplinary practice, requiring social, behavioral, and contextual information from the patient in order for the physician to make an informed decision about possible treatment.
The one-to-many relationship
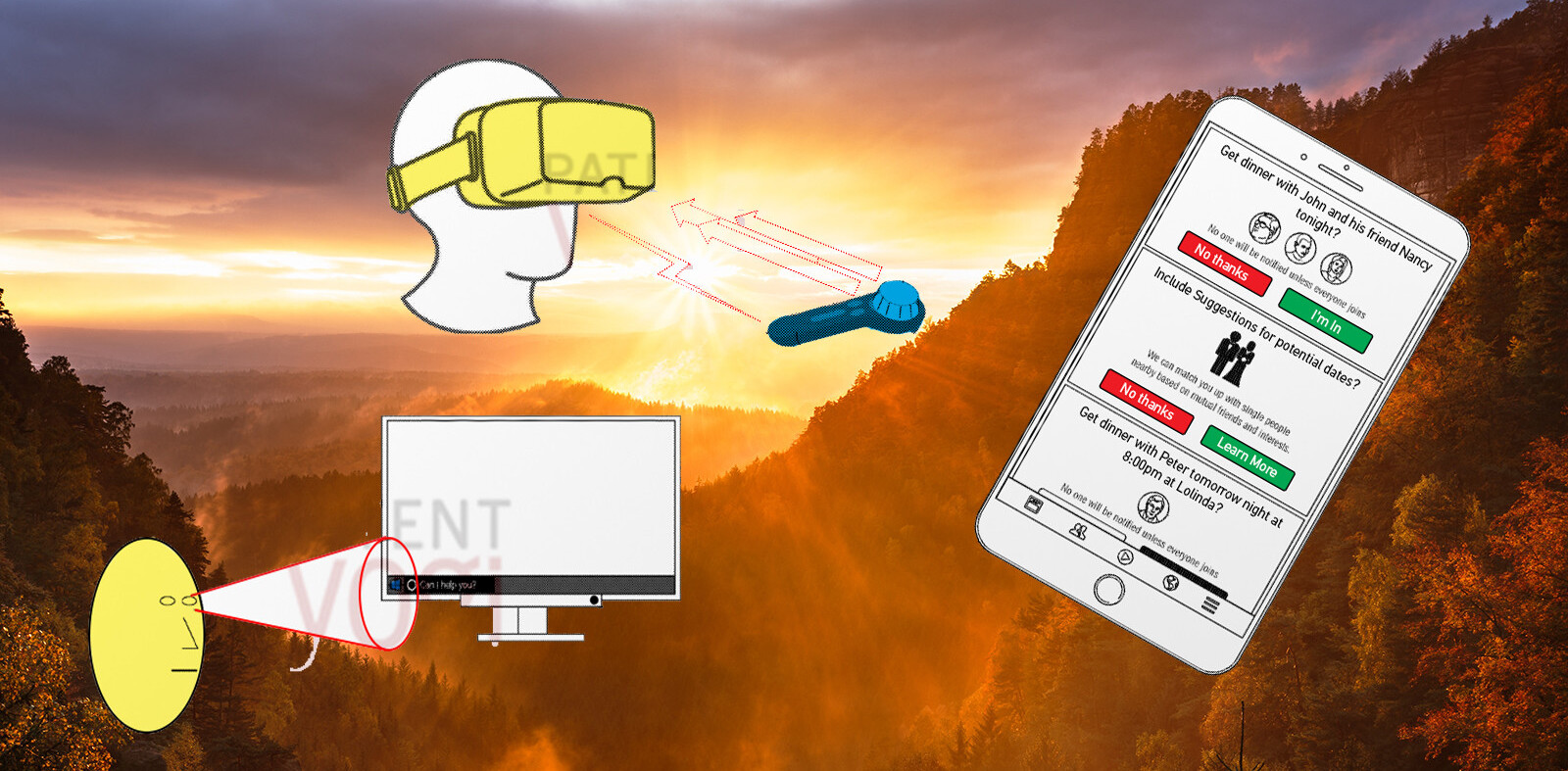
What does the future look like? I believe it starts with rethinking how we view the doctor-patient relationship. This relationship, at the foundation of modern medical practice, has traditionally been thought of as one-to-one, and this has to change. Our populations are aging around the world, putting pressure on healthcare budgets to deliver a quality standard of care. The one-to-one doctor-patient relationship is no longer sustainable.
Instead we should look to AI, machine learning, and modern communications technology to distribute physicians’ time more efficiently. Clinical teams can be augmented with AI technologies to automate more repetitive or non-critical tasks, such as supervising exercises, or analyzing test results. Rather than leading to job losses, this would free up more time for doctors and therapists to focus on delivering the unique value they have to offer.
Our healthcare future is bright, and it doesn’t involve robot doctors. Instead, we’ll see more patients assigned to a single doctor or physician, and technology will enable that one-to-many relationship to happen without significantly impeding on quality of care.
Get the TNW newsletter
Get the most important tech news in your inbox each week.