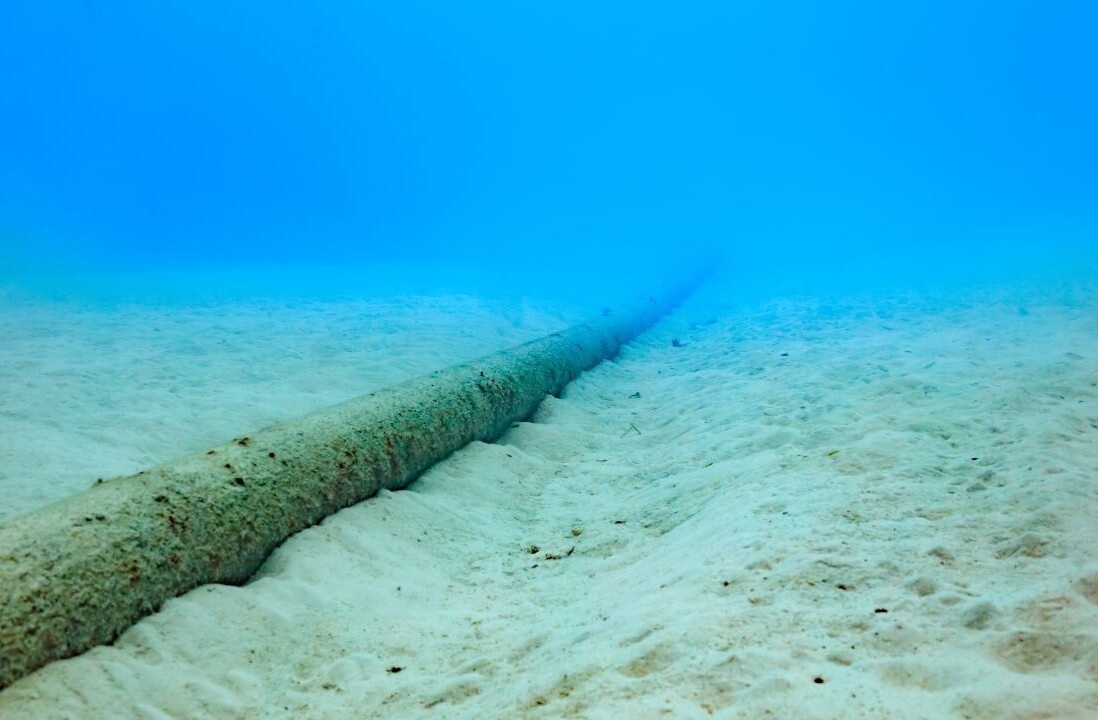
The issues faced by many in the healthcare industry when it comes to digitization are vast, not only in the UK and Europe but globally. We’ve come to view mobile phones as something we can take with us anywhere through the power of roaming. The same cannot be said for the delivery of wireless medical devices and networks, which could provide life-changing treatments to people, especially those with chronic conditions.
For example, in England, 15 million people suffer from long-term conditions, with their treatment absorbing 70 percent of acute and primary care budgets in the country. By 2018, the number of people with three or more long-term conditions is expected to hit 2.9 million, resulting in an extra £5 billion a year spend for the government.
In the United States, the Centers for Medicare and Medicaid Services (CMS) estimate that over 68 percent of its beneficiaries are afflicted with two or more chronic conditions. It is also noted that 70 percent of deaths are caused by chronic disease.
Even though the problem is real and technology is out there to help solve it, the digital transformation of healthcare isn’t picking up. Pilots have been launched across Europe and the United States, such as Qualcomm Life teaming up with TBS in the UK.
In the United States, Royal Philips and Arizona-based Banner Health have shown significant decreases in both patient health care costs and hospitalization rates. The World Economic Forum planned pilot programs in 2017 to show the value of a new model for health care that would track and pay for treatment based on how well it works rather than the volume of care.
Larger scale deployments are nowhere to be found
“In Europe, and other markets, there is a growing observation of low scalability of digital health and care approaches from pilots to large-scale deployment and widespread uptake,” Nathalie Vandystadt, European Commission Spokeswoman for the Digital Single Market, told BDJ.
“Despite the recognized potential of the digital transformation of health and care providers and integrated, person-centered care models, benefits have not come to fruition in many cases as initiatives remain at project stage and do not permeate health and care provision at scale.
“Implementing such innovations at a large scale, to offer services to all citizens who can benefit from them is a major challenge.
“The technology itself is no longer the problem in this regard. Rather, it is organizational issues such as commitment from authorities, the need to re-configure services, new patient pathway designs, new roles and skills for health and social care professionals, interoperability, privacy and data protection, sustained investments and new governance, contracting and payment schemes. In addition, according to a World Health Organization report (2016), the lack of funding is one of the most significant barriers to the deployment of digital solutions in health.”
Find funding fast
With the UK government pledging £20 billion to fund the NHS over the next six years, Europe investing in health care companies under Horizon 2020 and the United States’ Food and Drug Association (FDA) focusing on digital health, is funding really the barrier?
According to the UK’s NHS, two of the main hurdles in providing care for long-term conditions are: fragmented care and not being considered in a whole system approach with social care and other services; and lack of information continuity, with care records not being accessed between settings.
Funding isn’t mentioned in regards to its model The Care House, though the UK government has committed to an extra £10 billion in capital funding over the parliament for investment in buildings, facilities and equipment.
In Europe, the Commission encourages closer cooperation between regional and national authorities to stimulate the development of the health technology sector. This includes supporting start-ups and small and medium-sized enterprises that develop digital solutions for person-centered care and patient-feedback.
Horizon 2020 and Horizon Europe are two examples of funding resources but they’re by no means the only ones; the European Investment Bank, EIT Health, and investor networks also encourage further digital innovation for health. This differs from the United States, where hospitals have a mixture of revenue streams and health care companies rely on grants and venture capitalist funding.
Innovation for all
As noted by Vandystadt, technology isn’t a major barrier either. Abbott is an example of a medical device manufacturer with footprints across the globe. Working in over 150 countries and with over 125 years of experience in its line of work, the company has created devices to help people with conditions such as diabetes, neuromodulation disorders and cardiovascular.
For Joel Goldsmith, senior director of digital platforms at Abbott Diabetes Care, the devices mean nothing without access: “Innovation without access doesn’t make a difference.
To be truly innovative we need to make new technology available and accessible to all of those who may need it. Our mission is to develop revolutionary technology that is approachable and accessible to all – because true innovation shouldn’t be a barrier to better health.
“It starts by giving each person greater access to and control over their personal health information, so it can be securely shared with other authorized stakeholders. For example, The United States is a highly developed market, but it also has a highly fragmented health care delivery system and a demanding regulatory environment.”
Solving fragmented data sharing
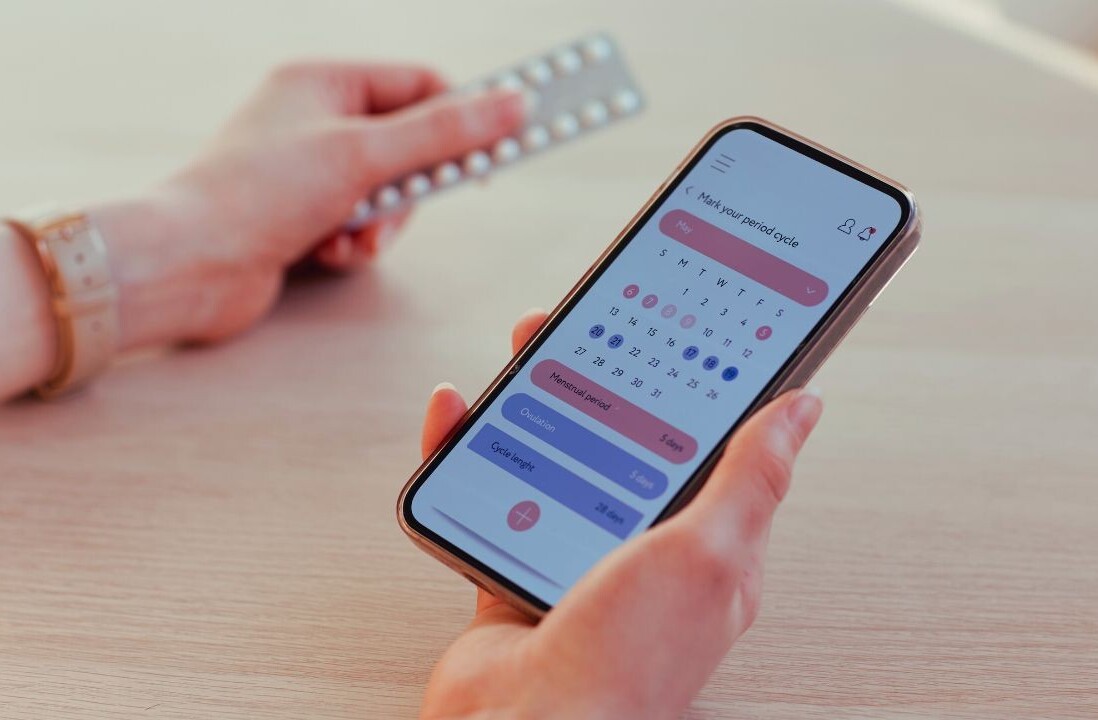
In our current healthcare industry, fragmentation and regulation cover data sharing. The health care sector has always dealt with large amounts of data, but now due to the experiential growth of wearable technology and health applications, more personal and real-time health data is available.
According to the mHealth App Economics 2017 study, there are more than 325,000 health apps currently available in major apps stores, but only 42 percent of consumers actually thought their healthcare providers were making effective use of the data available to deliver better care.
In the UK, only 26 percent thought their healthcare providers were making use of their data, compared to 54 percent in the United States, showing the difference between public and private health care environments.
Research has also suggested that the ability of healthcare professionals to access or share information effectively is impacting patient care. As a direct result of a lack of integration and efficient data-sharing methods, more than half of consumers said they, or someone they know, had experienced a delay in receiving care.
If this resulted in operations being cancelled due to patient notes being inaccessible or test results being delayed, it would result in funding being wasted, no matter if it was a public or private healthcare service.
Paul Cooper, Professional Adviser at The Royal College of Occupational Therapists, believes that technology is a good thing for healthcare systems, but there are drawbacks when it comes to data: “The Kings’ Fund recent reports sums up the main issues as the following; key barriers to successful digital change include the constraints care organizations face in their workforce, tight budgets, organizations’ attitudes towards risk and the relationships that exist between care providers and key stakeholders.
“Funding is one issue but as pointed out there are other issues around risk, attitudes and differing systems. Occupational therapists work across health and social care and there are challenges given each area which uses a different system to input data.
“We hear about staff working with older systems in their day-to-day working life. We have been calling for significant investment in an integrated IT system, as without it health and social care integration will fail.”
The FDA has had its say
In the US, the FDA has created guidelines to help companies navigate passing regulation if they were not creating software that actively monitors patient data. In an article for the JAMA Network, ‘FDA Regulation of Mobile Medical Apps’, author Jeffrey Shuren, MD, JD, US Food and Drug Administration, wrote: “After careful consideration, the agency has released guidance that makes it clear that not all these tools are subject to FDA regulation.
“The agency oversees most mobile apps that are intended to treat, diagnose, cure, mitigate, or prevent disease or other conditions as medical devices under federal statute. Not all mobile apps meet these characteristics.
“But for devices evaluated, the policies must continue to empower patients and clinicians and facilitate innovation, including by creating regulatory frameworks that give patients and clinicians confidence in the app’s performance and reliability.”
This need for regulation not only removes issues surrounding data protection and cyber-security, it also gives consumers confidence in the devices that they’re using. The steps by the FDA has also helped more companies move into the healthcare industry, such as Microsoft, Samsung and Apple.
Roger Cepeda, JD, MBA, and attorney at Health Sciences Law Group LLC, wrote that: “Whether [companies] are an incumbent, a contender, or a hopeful, the direction of FDA regulation in this area is positive.
Since the first iPad was launched, several types of healthcare software have moved from regulated to not regulated, and FDA’s guidance documents confirm that they intend to focus their enforcement resources on high-risk software products.
“If companies design their products in ways such that they are fairly described as not ‘active’ or not ‘primary,’ then the five ‘non-medical device’ categories of the Cures Act will become the standard way to consciously and lawfully avoid FDA regulation. This includes medical device data systems and mobile health apps.”
Working models
Cooper highlights that his sector is also seeing innovations to tackle this problem. MindWell, which resulted from a 2013 report written by users of mental health services, highlighted serious issues with accessing information. From this, Alicia Ridout, an occupational therapist in the Leeds and York Partnership NHS Foundation Trust, began building an integrated co-designed mental health information portal for Leeds.
The aim was to deliver the portal within a 12 month period, in close partnership with citizens, clinicians, carers and organisational partners across the city of Leeds, providing an effective, web-based resource that meets the needs of key users.
Alicia led the team that worked to engage all parts of the community in Leeds and listens to their views, ideas and requirements. MindWell information is carried by police and other front-line staff ensuring access and clear information, and a further 18-month schedule of content development is planned.
On the continent, the project APOLLON – funded under the Competitiveness and Innovation Framework Programme – demonstrated that for small to medium enterprises (SMEs) cross-border pilots forced them to re-think the initial business case into a European context.
This new approach increased the development process for building the right proposition and a better product fit, which had a huge impact on how they are currently developing and deploying the products and services.
“Cross-border exchanges give SMEs the opportunity to discuss the healthcare ecosystem in other countries,” Nathalie Vandystadt told us.
“This enables them not only to identify different needs and possible enhancements to their products but also to explore new business opportunities and give insight into the requirements and operational issues related to transferring products to other markets outside the base market.
“In the context of the Digital Single Market, it is critical to work towards the capacity of all Member States and regions to create value through novel approaches to health and care delivery. It can also be an opportunity to tackle differences in the effectiveness of the market for digital health and care provision, especially in the case of expenditure and spending patterns.”
For example, Eurostat data shows large differences in long-term care expenditure in Member States, between 4.0 percent of GDP in Finland and 0.01 percent in Bulgaria.
“While there is no linear relationship between healthcare expenditure and achieving health outcomes, and digital transformation does not intend to close gaps in healthcare spending, digital solutions can help health and social care systems achieve more with the resources available,” she continued.
So, as digital services continue to be created and piloted, there is a clear need for fragmented data systems to be streamlined, IT systems to be updated for the people working within the healthcare industry, and commitment from authorities to bring in the technology that is on offer.
“The countries that have the greatest healthcare related challenges are dealing with more basic access issues such as sufficient numbers of qualified health care professionals and basic infrastructure,” said Goldsmith. “For them, digital health is an important consideration, but only after the basic access issues are addressed.”
This post was written by Margarita Khartanovich for Binary District, an international collaborative technology community which creates unique competency-based workshops and events on new technologies. Follow them down here:
Get the TNW newsletter
Get the most important tech news in your inbox each week.