Robert J. Szczerba is the CEO of X Tech Ventures, an innovative company focused on solving some of today’s most challenging problems through the integration of technologies from multiple, diverse domains. This post originally appeared on Forbes.
More than 20 percent of Americans regularly consume prescribed drugs related to mental health issues, earning contemporary America the nickname, “the Prozac Generation.” However, developing safe, targeted, and effective drugs for mental illnesses has increasingly become a struggle for the pharmaceutical industry.
As a result, there’s been a gradual withdrawal of research dollars from this area, despite the fact that globally, the mental health pharmaceutical market is worth more than $80 billion.
According to the National Institute for Mental Health (NIMH), more than 57 million people, or 26 percent of the U.S. population suffer from some form of mental health problem. But despite the ongoing need, one can legitimately claim that research has not produced a novel neurological drug in the past 30 years. Additionally, many drugs currently on the market have been increasingly identified with negative side effects and limited efficacy.
Until recently, most mood disorders were attributed to an imbalance in a single neurochemical, such as serotonin. Increasingly, scientists have come to acknowledge that this is an oversimplification that can lead to counterproductive treatment.
Due to the complexity of brain networks, these pharmaceutical compounds may work to alleviate some symptoms, but they may exacerbate others. They may even contribute to new problems, such as cognitive impairment, suicide, or diabetes. Because the diagnosis of many conditions is a highly subjective process based on patient self-reporting, identifying the appropriate course of treatment is frequently an exercise in trial and error.
High cost, negative press, and the lack of an efficacy model have resulted in the drying up of the drug pipeline for pharmaceutical treatment of mental illness.
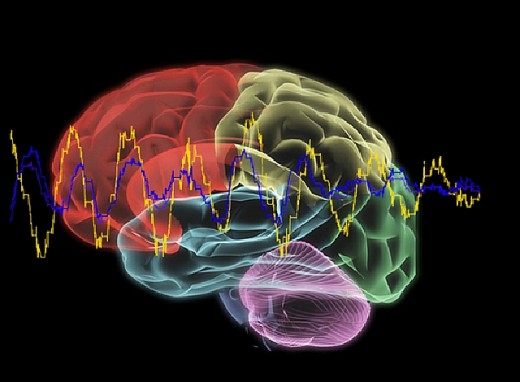
New technology and an increased focus on traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD), have led to a greater understanding of the complexity of the brain. Instead of focusing on single chemical neurotransmitters affecting cognition and behavior, mental health research has evolved to address neurological “functions” through models of neural circuits known as “neural networks.”
These functional brain regions can be influenced using non-invasive technologies such as brain-computer interfaces (BCI) and brain training. Many scientists see this movement towards identifying and modifying neural networks as a more effective and safer way to assess and treat problems related to cognition, behavior, and emotion.
A brain-computer interface is a direct communication pathway between the brain and an external device with the purpose of assisting, augmenting, or repairing cognitive and/or motor functions. The computer measures electrical activity in the brain by means of an electroencephalogram (EEG) and interprets the signals for display.
All of us produce a variety of electrical wave patterns that reflect what our brain is doing at any given time. These patterns can be compared to age-matched reference databases and/or to pre-treatment measurements of an individual to identify dysfunctional networks.
Brain training is the use of a brain-computer interface to learn to treat the dysfunctional networks and re-regulate cognitive and mental functioning. Through brain training, the individual can learn to control the specific dysfunctional network, essentially teaching the brain to function more efficiently (as shown in the video below).
The brain processing speed for vision, hearing, attention, thinking, and remembering can be measured in milliseconds. While BCI technology exists to perform these measurements and analysis, it has, until now, required advanced training to operate and understand. Therefore, the implementation of BCI has been mostly limited to research facilities staffed with biomedical engineers and neuroscientists. Ease-of-use has been a major limiting factor.
One intriguing response to this limitation comes from a company called Evoke Neuroscience. Founded by Drs. David and Nicole Hagedorn and Dr. James Thompson, Evoke has developed new “brain training” technologies to allow individuals to quickly and easily capture brain information. Their approach leverages wireless data-capture technologies, signal processing algorithms, cloud-based data storage and processing, and wearable biosensors.
As brain and other biometric measures are obtained, rapid analysis of the information is converted into graphical displays of the individual’s cognitive, emotional, and stress states. Cloud-based computing allows for near real-time display and analysis of the results.
According to Evoke CEO David Hagedorn, “the system allows doctors to quickly measure the brain and then safely modulate certain regions using any number of scalp sensors and patterns to remedy troubling symptoms.” If a deviation is detected, the problem area can be targeted with different forms of non-invasive treatment.
One approach is the use of transcranial direct current stimulation (tDCS), a form of neuro-stimulation using constant, low current delivered directly to a specific area of the brain via small electrodes. tDCS has been successfully utilized to enhance language skills, mathematical ability, attention span, problem solving, memory, and coordination.
“What is particularly promising about the use of brain interface technology,” Hagedorn continued, “is its efficacy not only in the treatment of mental illness but also in assessing and treating the physiological underpinnings of Parkinson’s, Alzheimer’s, concussion, traumatic brain injury, ADHD, and even the normal cognitive decline associated with aging.”
Recently, several brain processes known to decline in early Alzheimer’s disease have been identified and categorized using Evoke’s technologies. They have revealed functional abnormalities and dysfunctional brain lobes prior to any behavioral symptoms, creating the potential for early interventions to delay cognitive decline.
The neuroscience technology sector continues to be highly profitable, with growth estimates for the brain training and cognitive assessment sector reaching up to $5 billion by 2015. If those estimates are accurate, it may indeed be time for America to say goodbye to the Prozac Generation and hello to personalized brain training.
Get the TNW newsletter
Get the most important tech news in your inbox each week.